Dressler’s Syndrome Causes, Symptoms, Diagnosis and Treatment
What Is Dressler’s Syndrome?
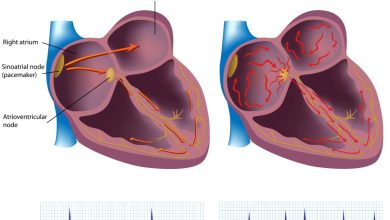
Dressler’s syndrome is a type of pericarditis – inflammation of the sac surrounding the heart (pericardium).
Dressler’s syndrome is believed to be an immune system response after damage to heart tissue or to the pericardium, from events such as a heart attack, surgery or traumatic injury.
Causes Of Dressler’s Syndrome:
Dressler’s syndrome is associated with an immune system response to heart damage.
The body reacts to the injured tissue by sending immune cells and proteins (antibodies) to clean up and repair the affected area. Sometimes this response causes excessive inflammation in the pericardium.
Dressler’s syndrome might affect 10 to 40 percent of people who have had heart surgery.
Presentation And Symptoms Of Dressler’s Syndrome:
Symptoms are likely to appear weeks to months after a heart attack, surgery or injury to the chest.
Symptoms might include:
- Chest pain
- Fever
Dressler’s syndrome presents itself in the following manner:
- It usually presents two to five weeks after the initial episode, with pain and fever that may suggest further infarction.
- The pain is the main symptom, often in the left shoulder, often pleuritic, and worse on lying down.
- There may be malaise, fever and dyspnoea.
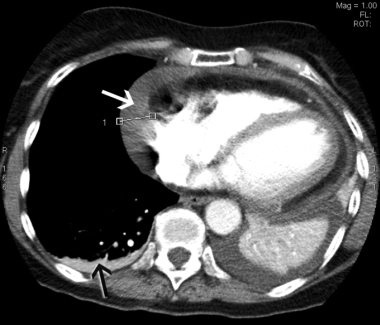
- Rarely, it may cause cardiac tamponade or acute pneumonitis.
- A pericardial friction rub may be heard
Diagnosis Of Dressler’s Syndrome:
The following tests are conducted in order to diagnose Dressler’s syndrome:
- Echocardiogram
- Electrocardiogram.
- Chest X-ray.
- Blood tests
Treatment For Dressler’s Syndrome:
The following medications help in treating Dressler’s syndrome:
- Aspirin may be given in large doses.
- Other non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be used, especially if there are severe and recurrent symptoms.
- Steroids are particularly valuable where severe symptoms have required pericardiocentesis, and when infection has been excluded.
- In resistant or recurrent cases, colchicine may be useful.
- If there is significant pericardial effusion then pericardiocentesis, involving aspiration of the fluid, may be required to relieve the constriction on the heart
Moreover, heparin should be avoided because it can lead to hemorrhage into the pericardial sac leading to tamponade. The only time heparin could be used with pericarditis is with coexisting acute MI in order to prevent further thrombus formation.
By : Natural Health News