A Surprising New Treatment for Rheumatoid Arthritis
Rheumatoid arthritis (RA) has long been one of the most challenging autoimmune conditions to treat. Characterized by chronic inflammation, pain, and progressive joint damage, RA affects millions worldwide and often reduces quality of life significantly. For decades, treatment options have primarily revolved around disease-modifying antirheumatic drugs (DMARDs), biologics, and corticosteroids. While these have brought relief to many, they are not without limitations — including side effects, high costs, and varying degrees of effectiveness.
But recently, research has unveiled a surprising new treatment approach for rheumatoid arthritis that is changing the way patients and doctors think about managing this complex disease. The latest breakthroughs, why they’re considered revolutionary, and how they could reshape the future of RA care.
Understanding Rheumatoid Arthritis
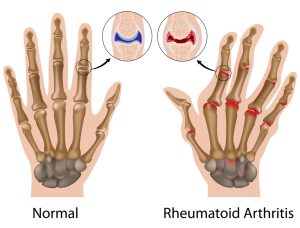
Before diving into the new treatment, it’s important to revisit what makes RA such a difficult disease to treat. Unlike osteoarthritis, which is primarily a wear-and-tear condition, RA is an autoimmune disorder. The immune system mistakenly attacks the synovium — the lining of the joints — leading to painful swelling, stiffness, and eventually joint deformity.
Some key characteristics of RA include:
- Chronic inflammation that doesn’t just affect joints but can also involve the lungs, heart, and blood vessels.
- Unpredictable flares where symptoms worsen suddenly.
- Progressive joint damage even in early stages of the disease.
- Significant impact on daily life, often leading to disability if untreated.
Traditional treatment strategies aim to reduce inflammation, suppress the overactive immune response, and prevent joint damage. Yet, even with biologics and targeted therapies, many patients continue to struggle. This has led scientists to search for alternative and more innovative solutions.
Related Article: Chronic Conditions – Diabetes, Arthritis, Asthma, Hypertension
Current Standard Treatments — and Their Limitations
To understand why the new treatment is so exciting, we need to look at where current therapies fall short.
- DMARDs (e.g., methotrexate, sulfasalazine)
- First-line treatments that slow disease progression.
- Limitations: side effects like liver toxicity, mouth sores, and gastrointestinal distress.
- Biologic agents (e.g., TNF inhibitors, IL-6 blockers, B-cell therapy)
- Revolutionized RA treatment by targeting specific immune pathways.
- Limitations: risk of infections, high costs, and patients may lose responsiveness over time.
- Corticosteroids (e.g., prednisone)
- Powerful anti-inflammatory effects.
- Limitations: weight gain, osteoporosis, diabetes risk, and long-term organ damage.
- NSAIDs (non-steroidal anti-inflammatory drugs)
- Provide symptomatic relief.
- Limitations: do not prevent disease progression, and long-term use increases cardiovascular and gastrointestinal risks.
Clearly, while these treatments help, the need for a safer, more sustainable, and more effective option is urgent.
Related Article: Juvenile Rheumatoid Arthritis Symptoms, Causes, Diagnosis and Treatment
The Surprising New Treatment for Rheumatoid Arthritis
The surprising breakthrough isn’t just a tweak to existing medications — it represents a fundamentally different approach. One of the most promising areas of recent research is microbiome-based therapy and vagus nerve stimulation, both of which shift the paradigm of how we understand RA.
1. Microbiome Therapy: Treating RA Through the Gut
Recent research has uncovered a powerful connection between gut health and autoimmune diseases like RA. The gut microbiome — trillions of bacteria living in the digestive tract — plays a critical role in regulating the immune system. Imbalances in gut bacteria, known as dysbiosis, have been linked to RA development and progression.
Surprisingly, scientists have found that modifying the gut microbiome can significantly improve RA symptoms. Some of the approaches being tested include:
- Probiotics and prebiotics: Certain strains of beneficial bacteria can reduce inflammation and restore immune balance.
- Fecal microbiota transplantation (FMT): Although still experimental, early studies suggest that transferring healthy gut bacteria into RA patients may help reset their immune system.
- Dietary interventions: Diets rich in fiber and polyphenols (e.g., Mediterranean diet) encourage anti-inflammatory gut bacteria growth.
One study from 2023 showed that RA patients who underwent targeted microbiome therapy experienced reduced joint swelling and improved mobility compared to those on conventional treatments alone.
Related Article: Rheumatoid Arthritis Diet: The Best Foods to be add
This has led many researchers to view the gut as the new frontier in rheumatoid arthritis treatment.
2. Vagus Nerve Stimulation: Bioelectronic Medicine for RA
Another surprising new treatment making headlines is vagus nerve stimulation (VNS), a form of bioelectronic medicine. The vagus nerve, which runs from the brainstem to the abdomen, helps regulate inflammation through what is known as the “inflammatory reflex.”
By using a small implantable device that delivers mild electrical impulses to the vagus nerve, researchers have successfully reduced inflammatory markers in RA patients.
Key findings include:
- Significant reduction in TNF (tumor necrosis factor), a major driver of inflammation in RA.
- Improvements in pain, joint swelling, and fatigue.
- A decrease in the need for traditional medications in some patients.
The most surprising part? VNS has minimal side effects compared to biologics or steroids, making it an attractive non-pharmaceutical option.
Related Article: Joint Support: Natural Joint Supplement for Arthritis Joint Relief Review
Other Emerging Surprising Therapies
In addition to microbiome therapy and vagus nerve stimulation, several other innovative treatments are showing promise:
- mRNA-based therapies
- Building on the technology behind COVID-19 vaccines, researchers are developing mRNA treatments to retrain the immune system and stop it from attacking healthy joints.
- Stem cell therapy
- Mesenchymal stem cells (MSCs) have shown anti-inflammatory and regenerative effects, potentially repairing damaged joint tissues.
- Targeted small-molecule inhibitors
- Janus kinase (JAK) inhibitors are already in use, but newer, more precise inhibitors may reduce side effects while keeping inflammation under control.
- Precision medicine
- Genetic testing and biomarker analysis can help tailor treatments to individual patients, improving effectiveness and minimizing unnecessary exposure to toxic drugs.
Why These Treatments Are Considered Surprising
What makes these treatments surprising is that they move beyond the conventional “drug-only” approach. Instead of just suppressing the immune system broadly, these methods target underlying mechanisms such as gut health, neural pathways, and cellular repair.
- They challenge the assumption that RA can only be managed with lifelong medication.
- They offer the possibility of fewer side effects compared to current therapies.
- They may provide more long-term remission rather than short-term symptom management.
For patients who have spent years cycling through medications with limited success, these new therapies represent a beacon of hope.
Related Article: Some Essential Foods to Eat in Rheumatoid Arthritis Diet
Patient Success Stories
The real-world impact of these surprising treatments is already being seen:
- Microbiome intervention: A 45-year-old woman with RA resistant to biologics reported significant improvement after participating in a gut-health clinical trial. Her morning stiffness reduced from 2 hours to just 20 minutes.
- Vagus nerve stimulation: In one European trial, over half of RA patients implanted with a VNS device achieved low disease activity within three months — without increasing their medication doses.
- Stem cell therapy: Patients in early trials reported improved joint mobility and reduced reliance on painkillers.
These success stories highlight the transformative potential of these novel approaches.
Challenges and Considerations
Despite the excitement, there are challenges:
- Cost and accessibility
- Bioelectronic devices and stem cell treatments can be expensive. Ensuring access will be a major hurdle.
- Long-term safety
- While short-term trials are promising, we need long-term data to confirm safety and sustained effectiveness.
- Regulatory approval
- Many of these therapies are still in experimental stages and require rigorous testing before becoming widely available.
- Integration with existing treatments
- Researchers are exploring whether these new treatments can replace current therapies or work best in combination.
The Future of Rheumatoid Arthritis Treatment
Looking ahead, the future of RA care may be a multi-pronged approach that combines traditional medications with these novel therapies. For example, a patient might use microbiome therapy to restore immune balance, vagus nerve stimulation to control inflammation, and low-dose DMARDs to maintain remission.
Related Article: New research could halt rheumatoid arthritis
In the next decade, it’s possible that RA treatment will shift from heavy reliance on pharmaceuticals to a more holistic, personalized model that includes gut health, bioelectronics, regenerative medicine, and precision diagnostics.
Practical Tips for Patients Right Now
While many of these treatments are still in development, patients can take steps today to support their health:
- Focus on gut health: Eat a fiber-rich diet with plenty of fruits, vegetables, and fermented foods.
- Stay active: Gentle exercise like swimming or yoga helps maintain joint flexibility.
- Manage stress: Stress worsens inflammation; mindfulness, meditation, or breathing exercises may help.
- Discuss new options with your doctor: If clinical trials are available in your area, consider whether participation could be beneficial.
Conclusion
Rheumatoid arthritis has long been viewed as a disease that requires lifelong medication and constant management. But with the rise of surprising new treatments like microbiome therapy, vagus nerve stimulation, and stem cell applications, we may be entering a new era of hope for patients.
These breakthroughs highlight the shift toward treating the root causes of autoimmunity rather than just symptoms. While challenges remain, the future looks brighter than ever for those living with RA.
For patients, the message is clear: the next generation of RA therapies may not come from a pill bottle, but from innovative science that harnesses the body’s own systems — gut bacteria, neural pathways, and regenerative cells — to heal itself.