FDA Approves New COVID-19 Shots – But Why Are Some Kids and Adults Left Out?
The U.S. Food and Drug Administration (FDA) recently approved updated COVID-19 vaccines designed to target newer strains of the virus. The move comes as health experts prepare for another respiratory virus season, where COVID-19, influenza, and RSV are expected to circulate simultaneously. While many hailed the approval as a timely step in boosting immunity, the decision also raised eyebrows: not everyone is eligible to receive these updated shots. Some children and even certain adults have been excluded from the recommendation, sparking debate and questions about safety, necessity, and equity.
We will explore what the FDA approved, why certain groups are left out, the scientific reasoning behind these exclusions, and what it means for families trying to make sense of evolving vaccine guidance.
Understanding the New FDA-Approved COVID-19 Shots
The newly approved vaccines are updated formulations of the mRNA shots originally developed by Pfizer-BioNTech and Moderna. Unlike the initial vaccines, which were based on the original strain of SARS-CoV-2 from Wuhan, the new versions are designed to target more recent variants, particularly the Omicron XBB.1.5 lineage and its subvariants. These strains have dominated , and scientists expect the updated vaccines to provide stronger protection against infection, hospitalization, and severe illness.
The FDA’s approval follows a similar seasonal vaccine approach used for influenza: update the formulation annually to better match circulating strains. This shift suggests that COVID-19 vaccinations may become a yearly routine, much like flu shots, especially for vulnerable populations.
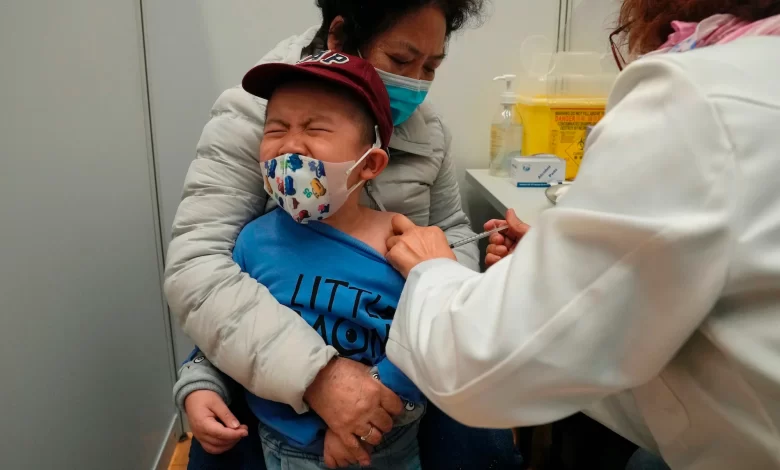
Why Are Some Kids Left Out?
Perhaps the most striking exclusion involves very young children—those under six months of age. While parents of infants may feel anxious about leaving their babies unprotected, there are several scientific reasons for this decision:
- Immature immune systems:
Babies under six months often do not respond strongly to vaccines. Their immune systems are still developing, making it difficult for vaccines to generate long-lasting protective antibodies. - Maternal antibodies:
Research shows that antibodies from vaccinated or previously infected mothers can pass through the placenta during pregnancy and through breast milk after birth. This natural transfer offers infants passive protection in their first months of life. - Clinical trial limitations:
Clinical trials for COVID-19 vaccines in infants have been limited, and regulators are cautious about authorizing widespread use without sufficient safety and efficacy data.
The combination of these factors explains why the FDA and CDC have excluded babies under six months from the new rollout. Instead, public health officials encourage vaccination during pregnancy to help protect newborns.
Why Are Some Adults Left Out?
On the other end of the age spectrum, certain healthy adults under 50 may also be left out of the latest recommendations. This may come as a surprise, especially since adults were the first priority group during the original vaccine rollout in 2021. Here’s why the guidance has shifted:
- Lower risk of severe illness:
Data shows that younger, healthier adults are much less likely to experience hospitalization or death from COVID-19 compared to seniors or immunocompromised individuals. - Waning demand and vaccine fatigue:
Uptake of boosters has dropped sharply over the past two years. Public health officials recognize that encouraging shots for the most vulnerable may be more impactful than pushing for universal coverage. - Immunity from past infections and vaccinations:
By 2025, a large portion of the U.S. population has either been vaccinated, infected, or both—often multiple times. This layered immunity means that most adults already have some level of protection, making annual boosting less critical for the general healthy adult population.
Thus, the FDA has prioritized high-risk groups—seniors, the immunocompromised, and those with chronic conditions—while giving younger adults more flexibility.
The Equity Dilemma: Access vs. Necessity
Leaving certain groups out of eligibility has sparked a debate over vaccine equity. Critics argue that restricting access could create confusion or even mistrust. Some parents want their children vaccinated regardless of age-based exclusions, while some healthy adults still desire extra protection.
On the other hand, experts argue that focusing resources on those most at risk makes sense from a public health perspective. Vaccines, after all, are not free to produce or distribute. By targeting the shots toward seniors, people with underlying health conditions, and young children above six months, the FDA aims to maximize impact.
The Science Behind Vaccine Updates
To understand the FDA’s decision-making, it helps to review how COVID-19 vaccines are updated and evaluated:
- Variant monitoring:
Global health agencies, including the World Health Organization (WHO), track dominant variants circulating worldwide. - Laboratory testing:
Scientists test whether existing vaccines produce strong neutralizing antibodies against new variants. If protection is weak, updated formulas are considered. - Clinical data:
For safety and effectiveness, manufacturers run small-scale trials using updated vaccines. Regulators then evaluate immune responses and side effects. - Expert advisory panels:
The FDA relies on advisory committees like the Vaccines and Related Biological Products Advisory Committee (VRBPAC) to review evidence and recommend action.
This process mirrors the one used for influenza vaccines each year, though COVID-19 remains less predictable in terms of variant evolution.
The Role of CDC Recommendations
While the FDA approves vaccines for use, the CDC ultimately issues guidelines on who should receive them. This distinction is critical: the FDA determines what is legally permissible, while the CDC determines what is medically advisable.
For example, even though the FDA has approved updated COVID-19 shots for broad age ranges, the CDC has recommended them primarily for groups most at risk. This sometimes creates confusion among the public—parents may hear that a shot is “approved” but not “recommended” for their child.
Clear communication remains a challenge, as health authorities balance scientific caution with public trust.
Parents’ Concerns: Protecting the Youngest
Parents of children under six months face a unique dilemma. They cannot vaccinate their infants directly, yet COVID-19 still poses some risk—even if lower than in older adults. Pediatricians suggest several strategies for parents in this situation:
- Vaccination during pregnancy: Pregnant women who receive the updated shot can pass protective antibodies to their babies.
- Breastfeeding benefits: Antibodies present in breast milk may help protect newborns.
- Reducing exposure: Families are advised to continue practicing reasonable precautions, especially during surges—such as avoiding crowded indoor spaces and ensuring caregivers are vaccinated.
These layered approaches help protect the youngest until they become eligible for their own shots.
Adults in the Middle: To Boost or Not to Boost?
For healthy adults under 50, the choice is more nuanced. Some may question whether getting another shot is necessary. Factors to consider include:
- Occupation: Healthcare workers, teachers, and service industry employees may want extra protection due to frequent exposure.
- Household risk: Adults living with elderly or immunocompromised relatives may choose vaccination to reduce transmission.
- Personal health history: Those with conditions like asthma and diabetes or heart disease fall into higher-risk categories regardless of age.
Ultimately, the decision for middle-aged adults often comes down to balancing personal risk tolerance with public health guidance.
The Bigger Picture: Living with COVID-19
The exclusions from the new vaccine rollout reflect a broader shift in how the U.S. is managing COVID-19. No longer treated as an unprecedented emergency, the virus is now being managed more like influenza: a recurring seasonal illness that poses the greatest danger to vulnerable groups.
This new approach acknowledges both scientific reality and public fatigue. Most Americans have been exposed to the virus in some form, meaning widespread natural immunity exists. Meanwhile, maintaining public compliance with yearly boosters for all age groups is unrealistic.
By focusing on high-impact populations, health authorities hope to reduce hospitalizations and deaths while allowing society to move forward.
Challenges Ahead
Despite careful planning, several challenges remain:
- Public confusion: Mixed messages about eligibility and necessity risk fueling skepticism.
- Misinformation: Social media amplifies doubts, especially among parents worried about safety.
- Equity of access: Low-income and rural communities may struggle to access shots even when eligible.
- Future variants: A sudden new variant could render current vaccines less effective, forcing another update.
These uncertainties highlight why flexibility and transparency are crucial in vaccine policy.
Looking Ahead: What Families Should Know
For families trying to navigate the latest guidance, here are some practical takeaways:
- Check eligibility carefully: The FDA approval covers broad groups, but CDC recommendations may narrow who should get vaccinated now.
- Consult healthcare providers: Pediatricians and family doctors can provide tailored advice, especially for children and those with chronic conditions.
- Vaccination during pregnancy matters: For infants too young to be vaccinated, maternal vaccination is the best line of defense.
- Expect yearly updates: Much like flu shots, COVID-19 vaccinations are likely to become an annual routine for many.
- Stay informed: Recommendations may change as new data emerges and as variants evolve.
Conclusion:
The FDA’s approval of new COVID-19 shots marks another step in the ongoing effort to adapt to a virus that refuses to disappear. While some may feel uneasy that certain children and adults are excluded from immediate eligibility, the reasoning is grounded in science: protecting those who need it most while avoiding unnecessary medical interventions.
For parents, the focus should be on maternal vaccination, breastfeeding, and reducing exposure for infants under six months. For younger adults, the decision to get boosted depends on personal risk factors and household circumstances. For seniors and vulnerable individuals, the message is clear: get the shot.
As the world transitions into a new phase of coexistence with COVID-19, the challenge for public health agencies will be maintaining trust, ensuring equitable access, and staying one step ahead of the virus. The story of the new vaccine rollout is not just about who can get the shot—it’s about how society learns to live with the enduring presence of COVID-19.




