Could Your Favourite Foods Be Making You Depressed? The Science Says Yes

When Comfort Food Becomes a Hidden Enemy
We all have those foods we crave—ice cream at midnight, sugary drinks to perk us up, fast food after a long day. They feel like comforts. But what if these indulgences—our “feel-good” foods—are secretly dragging you down emotionally? What if the very foods you turn to for solace are fueling deeper sadness, mood swings, or even depression?
There’s growing scientific evidence that what we eat doesn’t just affect our waistline—it affects our brain chemistry, mood regulation, and mental health. We’ll explore how favourite foods may be influencing your emotional state, what science has found, and what you can do to protect your mind as well as your body.
The Sugar Spike and Mood Crash: More Than Just a Guilt Trip
Sugar’s Role in Depression Risk
Sweet treats, sodas, refined carbohydrates—these are high in added or free sugar. A large meta-analysis (40+ studies, over 1.2 million people) found that higher sugar intake is associated with about a 21% increased risk of depression.
Another prospective study—Whitehall II—showed that people in the highest division of sugar intake from sweets & sugary drinks had significantly higher odds (~23%) of developing common mental disorders 5 years later.
What Happens in Your Body and Brain After Sugar
- Blood sugar swings: A sugary food causes a rapid spike in blood glucose, releasing insulin, then often a crash. That crash can make you feel tired, irritable, and anxious. Over time, these fluctuations stress your system.
- Inflammation and oxidative stress: High sugar diets can increase inflammatory markers like IL-6, TNF-α. Chronic inflammation is increasingly linked to depressive symptoms.
- Gut-Brain Axis Disruption: Sugar affects the balance of gut bacteria. This microbiome shift might influence mood via the gut-brain communication, producing or failing to suppress molecules that impact the brain.
Ultra-Processed Foods: The Hidden Triggers
Foods that are ultra-processed (fast foods, ready meals, sweetened snacks, pre-packaged baked goods) often carry multiple risk factors for depression:
- High sugar
- Refined carbs
- Artificial additives and sweeteners
- Low nutrient density
A study from the U.S. followed over 30,000 women who initially did not have depression. It showed that those who ate nine or more servings of ultra-processed foods each day had nearly a 49% greater risk of developing depression, compared to those eating fewer than four servings.
Even cutting down by a few servings per day corresponded to reduced depression risk. The pattern is strong, though causation (cause-and-effect) is still being explored.
Obesity, Insulin Resistance, and Emotional Toll
Often intertwined with diet is body composition and metabolic health.
- Obesity itself is strongly linked with depressive symptoms. In obese people, high sugar intake correlates with more frequent depression. Part of the reason: inflammatory pathways are more active in obesity.
- Insulin resistance (when glucose is poorly handled) can lead to higher blood sugar swings, oxidative stress, and hormonal dysregulation—including those hormones that manage mood, like cortisol. These can amplify emotional distress.
Do “Good Fats,” Whole Foods, and Micronutrients Help Protect You?
It’s not all doom and gloom. While some foods seem to increase risk, others may help shield the brain.
Omega-3 Fatty Acids
- Many observational studies find that people who consume more omega-3-rich foods (fatty fish, flaxseeds, walnuts) tend to have lower rates of depression.
- However, clinical trials where omega-3 supplements were given to prevent depression in healthy adults show mixed or weak evidence. Some trials show little to no preventive effect in people without depression.
Whole Foods, Fiber, and Plant-Based Diets
- Diets that emphasize vegetables, fruits, legumes, whole grains, and lean proteins tend to have lower levels of inflammation and better mood outcomes. Real, unprocessed foods carry micronutrients—vitamins, minerals, polyphenols—that help with brain function and emotional stability.
Is It Really Food or Just Feelings? Considering Reverse-Causality
One challenge in interpreting these studies is directionality. Does eating sugar cause depression, or do depressed people tend to eat more sugary comfort foods?
- Some long-term prospective studies try to handle this by controlling for baseline mood, lifestyle, socioeconomic status, etc. For example, the Whitehall II study followed people over years and found sugar intake predicted later mood disorders, even after adjusting for prior mood.
- Still, psychology is complex: stress, genetics, and personal habits all intermix. Food is one piece of the puzzle, not the sole culprit.
What to Do: Small Steps to Protect Your Mind
The good news: small dietary changes can make a difference.
| Change | Why It Helps | How to Begin |
| Cut down added sugar & refined carbohydrates | Reduces blood sugar spikes, inflammation, and mood roller-coasters | Swap soda & sugary drinks for water/unsweetened alternatives; choose whole grains instead of white bread, pasta, sweets |
| Reduce ultra-processed and packaged foods | Less artificial additives, more real nutrients | Cook more at home; read labels; choose minimally processed snacks (nuts, fruit) |
| Increase whole-food sources of healthy fats & micronutrients | Supports brain health, hormone balance | Include oily fish, seeds, and nuts; eat leafy greens, berries, and vegetables |
| Keep an eye on portion & timing | Even “good” foods can overload metabolic systems if misused | Balanced meals (protein + fiber + healthy fat) that sustain stable energy |
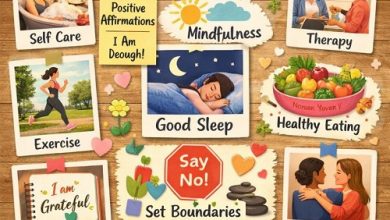
| Lifestyle complements diet | Sleep, exercise, and stress all affect mood | Ensure enough sleep, regular exercise, mindfulness, and social connection |
Real Stories, Real Change
Imagine waking up each day feeling foggy, lethargic, emotionally overwhelmed—and each bowl of sugary cereal, each fast-food dinner, each snack feels like a momentary escape that leaves a deeper crash. These are stories countless people live without realizing that food plays a silent role.
But then change: swap sugary breakfast for oatmeal with berries, drink tea instead of soda, cook simple meals, notice energy is more stable, mood is less volatile. It’s not overnight, but over weeks, many report feeling more mentally resilient, less anxious, and more hopeful.
Conclusion: Food as Mood Medicine
The science is growing clear: your diet—especially your favourite but “comfort” foods—can play a powerful role in your emotional life. While they might feel good briefly, over time, foods high in sugar, ultra-processing, and refined carbs may undermine mood, stability, and even increase depression risk.
It’s not about perfection or denying every pleasure. It’s about becoming aware, making small shifts, choosing foods that heal rather than hurt, so your body and brain both feel nourished. Because in many cases, food can be medicine—for your mind.