Effective Natural Remedies for Sjogren’s Syndrome The Power of Nature

Understanding Sjogren’s Syndrome and Its Impact on Daily Life
Sjogren’s Syndrome is an autoimmune condition that affects millions of people worldwide. It primarily targets the body’s moisture-producing glands, leading to chronic dryness of the eyes, mouth, and other mucous membranes. It can significantly impact daily life, causing discomfort, pain, and difficulty performing everyday tasks. While traditional treatments for Natural Remedies for Sjogren’s Syndrome focus on managing symptoms, they often come with limitations and side effects. As a result, many individuals are turning to Natural Remedies for Sjogren’s Syndrome as a complementary approach to alleviate their symptoms and improve their overall well-being.
The Limitations of Traditional Treatments for Sjogren’s Syndrome
Traditional treatments for Sjogren’s Syndrome include medications such as artificial tears, saliva stimulants, and immunosuppressants. While these treatments can provide temporary relief, they often fail to address the condition’s underlying causes. Additionally, they may come with unwanted side effects, such as blurred vision, upset stomach, and increased susceptibility to infections. Furthermore, these treatments do not offer a holistic approach to managing Sjogren’s Syndrome, leaving individuals searching for alternative options.
Exploring The Effectiveness of Natural Remedies for Sjogren’s Syndrome
Natural Remedies for Sjogren’s Syndrome have gained popularity among individuals seeking alternative ways to manage their health conditions. Regarding Sjogren’s Syndrome, several Natural Remedies for Sjogren’s Syndrome have shown promise in alleviating symptoms and improving overall quality of life. These remedies focus on nourishing the body, reducing inflammation, and supporting the immune system. By harnessing the power of nature, individuals with Sjogren’s Syndrome can find relief from dryness and discomfort without the unwanted side effects often associated with traditional treatments.
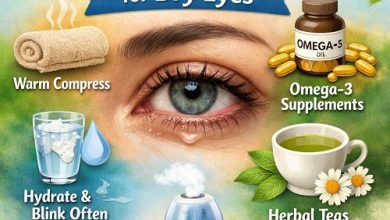
Key Natural Remedies for Managing Dry Skin Associated with Sjogren’s Syndrome
Dry skin is a common symptom experienced by individuals with Sjogren’s Syndrome. Several key remedies can be incorporated into a daily skincare routine to combat this issue naturally. One effective remedy is applying aloe vera gel, which has moisturizing and soothing properties. Another option is using coconut oil, which can help to lock in moisture and reduce inflammation. Additionally, incorporating omega-3 fatty acids into the diet through fish oil supplements or foods like salmon and flaxseeds can support skin health and hydration.
Incorporating Herbal Remedies to Alleviate Sjogren’s Syndrome Symptoms
Herbal remedies have long been used in traditional medicine to address various health conditions. When managing symptoms of Sjogren’s Syndrome, certain herbs can relieve and support overall well-being. For instance, chamomile tea can help to soothe dry and irritated eyes, while liquorice root has anti-inflammatory properties that can reduce discomfort in the mouth and throat. Additionally, herbs such as turmeric and ginger can be beneficial due to their potent anti-inflammatory effects. Incorporating these herbal remedies into daily routines can complement traditional treatments and provide additional relief for individuals with Sjogren’s Syndrome.
The Role of Diet and Nutrition in Managing Sjogren’s Syndrome Naturally
Proper nutrition plays a crucial role in managing Sjogren’s Syndrome naturally. Including foods rich in antioxidants, such as berries, leafy greens, and colourful vegetables, can help reduce inflammation and support overall immune function. Additionally, staying hydrated is essential to counteract the dryness associated with the condition. Drinking plenty of water and consuming hydrating foods like cucumbers and watermelon can help maintain moisture levels in the body. Moreover, avoiding trigger foods, such as caffeine, alcohol, and processed foods, can minimize symptoms and improve overall well-being.
Lifestyle Changes to Support Overall Well-Being and Symptom Relief
In addition to incorporating Natural Remedies for Sjogren’s Syndrome and dietary changes, certain lifestyle modifications can greatly contribute to managing Sjogren’s Syndrome effectively. Regular exercise, such as yoga or low-impact activities, can help reduce inflammation, improve circulation, and enhance overall well-being. Adequate rest and stress management techniques, such as meditation or deep breathing exercises, can also significantly relieve symptoms. Furthermore, protecting oneself from environmental factors that may exacerbate symptoms, such as extreme temperatures or dry air, is important. Individuals with Sjogren’s Syndrome can support their overall health and experience improved quality of life by making these lifestyle changes.
Precautions And Considerations When Using Natural Remedies for Sjogren’s Syndrome
While natural remedies can effectively manage Sjogren’s Syndrome, it is crucial to approach them cautiously and seek guidance from healthcare professionals. Certain herbs and supplements may interact with medications or have contraindications for specific individuals. It is essential to discuss the use of natural remedies with a healthcare provider to ensure safety and effectiveness. Additionally, it is important to remember that natural remedies may only work for some, and individual results may vary. It is always advisable to start with small doses and monitor any changes or reactions before fully incorporating Natural Remedies for Sjogren’s Syndrome into a routine.
Success Stories: Real-Life Experiences with Natural Remedies for Sjogren’s Syndrome
Many individuals with Sjogren’s Syndrome have found relief and improved their quality of life through natural remedies. These success stories serve as inspiration and motivation for others seeking alternative options. By sharing personal experiences, individuals can learn from one another and gain insights into which natural remedies may work best for them. It is important to note that what works for one person may not work for another, as each individual’s body and condition are unique. However, these success stories highlight the potential benefits of Natural Remedies for Sjogren’s Syndrome and provide hope for those looking to manage Sjogren’s Syndrome effectively.
Conclusion: Embracing the Power of Nature in Managing Sjogren’s Syndrome Effectively
In conclusion, natural remedies offer a complementary approach to managing Sjogren’s Syndrome, relieving dryness and discomfort while supporting overall well-being. By understanding the limitations of traditional treatments and exploring the potential of natural remedies, individuals can unlock the power of nature in their journey towards managing Sjogren’s Syndrome effectively. Incorporating key remedies for dry skin, herbal remedies, and a nutritious diet can significantly improve symptom relief. Additionally, lifestyle changes and precautions should be considered to optimize results and ensure safety. With the support of healthcare professionals and the inspiration of success stories, individuals with Sjogren’s Syndrome can embrace the power of nature and improve their quality of life.