Oura Labs Teases Groundbreaking Blood Pressure Study — Here’s What to Expect!
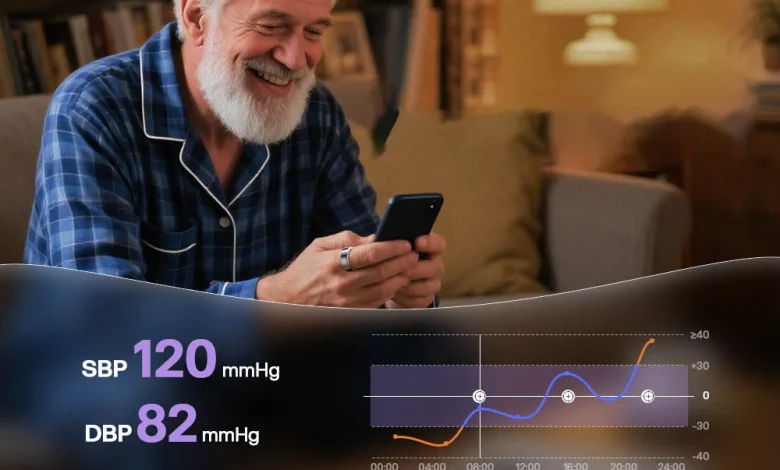
In an era where consumer wearables are rapidly evolving from fitness trackers into serious health-and-wellness tools, the Finnish smart-ring maker Oura is making waves again. The company behind the popular Oura Ring 3 (and most recently the Ring 4) has now announced a new initiative: a study named the Blood Pressure Profile Study, designed to explore how their device and software might help identify early signs of hypertension.
What exactly does this mean? What are the implications for users, for wearable health-tech more broadly, and for how we monitor cardiovascular health moving forward? In this article I’ll dig into:
- Why this matters — both for Oura and for you
- What we know so far about the study and how it works
- What to expect from the outcomes (positive, negative, neutral)
- How this fits into the bigger picture of wearables & blood pressure monitoring
- What you (as a user) should keep in mind and watch out for
Let’s get into it.
Why this matters
Hypertension: the silent health crisis
Hypertension — or high blood pressure — is among the most common and most under-recognized health risks worldwide. According to Oura’s own blog post, “an estimated 46% of adults with hypertension are unaware that they have it, while only 1 in 5 adults with hypertension are managing the condition effectively.”
That’s important. Why? Because blood-pressure elevation often doesn’t manifest obvious symptoms until more severe cardiovascular damage has occurred. Wearable technology has long sought to detect subtle signals earlier, and if a device you already wear (e.g., your Oura Ring) can help flag risk, that can be a major shift in preventive health.
Oura’s shift: from recovery tracker to cardiovascular sentinel
Oura’s brand has primarily centered on sleep tracking, readiness, activity, and recovery. But this announcement signals a step into deeper cardiovascular monitoring. Their press release states they aim to “translate quiet signals into clear, actionable insights” and to help “people stay ahead of potential issues” by combining wearables with research-grade measurement.
In other words: Oura is evolving from passively tracking your sleep and HRV (heart-rate variability) toward trying to assess a condition like hypertension — which places it more squarely in the realm of health-tech rather than purely lifestyle tech.
Competitive & regulatory context
This move also positions Oura in direct competition with other wearable players offering (or seeking) blood-pressure or hypertension detection features. For example, the Apple Watch recently received FDA clearance for a hypertension notification capability.
Moreover, Oura has stated explicitly that the Blood Pressure Profile Study is IRB (Institutional Review Board) approved and links to regulatory (FDA) efforts.
So, the significance is two-fold: one, from a health-impact standpoint; two, from a wearable-industry/consumer-tech standpoint.
What we know about the study
Although full detailed data aren’t yet publicly available — the study is forthcoming — we can summarise what Oura has announced so far.
Eligibility and mechanics
From sources:
- The study is available through “Oura Labs,” Oura’s experimental/early-access research platform.
- It requires participants to be United States-based, 22 years or older, using an Oura Ring Gen 3 (or newer) and the English version of the Oura app. Pregnant individuals, those within 12 weeks postpartum, and those with cardiac implants (e.g., pacemakers) are excluded.
- The study does not require traditional upper-arm cuff measurements or doctor-office visits. Rather: wear your Oura Ring as usual, answer some background questions (family history, medications, lifestyle), and Oura uses its sensors + questionnaire responses to estimate the likelihood of hypertension risk.
What the output looks like
- Participants will receive a risk assessment categorised into “No signs”, “Moderate signs”, or “Major signs” of hypertension risk.
- If the algorithm detects “strong signs,” participants will be encouraged to seek professional medical care.
- The algorithm is designed to track changes over time — so it’s longitudinal rather than a one-time snapshot.
Scope & positioning
- The study is described as “investigational” and is part of Oura’s larger preventive-health ecosystem. Importantly, Oura clarifies that the device is not a medical device and the feature is not meant to diagnose, treat, or monitor medical conditions on its own. From the press release: “Oura Ring is not a medical device and is not intended to diagnose, treat, cure, monitor or prevent medical conditions or illnesses.”
- They are engaging with regulatory pathways (FDA) in parallel, suggesting that eventual feature rollout (beyond the study) may subject to clearance.
Timing
- The announcement states participation is “in the coming months” for U.S. members of Oura Labs.
- The app redesign containing related features (Cumulative Stress metric) will roll out globally first, but the blood-pressure study is U.S.-based initially.
What to expect — and what to temper your expectations with
Given the above, here are some likely outcomes and caveats to keep in mind as the study proceeds, and as future features may roll out.
The potential positive outcomes
- Early detection / risk flagging: If the algorithm works reliably, wearers could receive early warning signals of elevated blood-pressure risk before they would otherwise realise it. That can lead to earlier lifestyle changes (diet, exercise, stress management) and clinical check-ups.
- Seamless monitoring: One of the appeals of ring-based monitoring is that it’s low burden — you wear it, go to sleep, and the sensors passively collect data. An ability to flag risk without having to purchase a new device or wear a separate monitor is attractive.
- Trend-based insights: Because the algorithm tracks over time, shifts in risk might be identified — for example, gradual drift upward, or detecting the impact of stress or poor sleep on cardiovascular strain. That could empower users with actionable insights: “Hey, your readiness is down, your recovery is poor, your ring is showing elevated stress and your BP-risk category just moved.”
- Data for research: Beyond individual benefit, the scale of data (if many users opt-in) may help build knowledge of how subtle physiological signals (HRV, temperature, sleep micro-motions) correlate with hypertension risk in real-world populations.
The caveats and limitations
- Not a conventional BP measurement: Oura makes clear this is not providing actual systolic/diastolic readings (at least initially). Bloomberg notes: “designed to detect early signs of hypertension … without displaying actual systolic or diastolic readings.”
- If you expect to replace your cuff device entirely today, that expectation would be premature.
- Algorithmic risk ≠ diagnosis: The output is about likelihood or risk category, not definitive diagnosis. Users with “major signs” are encouraged to seek medical care — but this doesn’t mean the ring replaces clinical measurement.
- Population and device limitations: The current study is U.S.-based and for Gen 3+ ring users only. So global users or those with older devices may have to wait. Also, the sample may not cover all demographic groups equally.
- Regulatory clearance is still pending: Until clearance is obtained, this remains investigational. That means feature rollout, accuracy, and clinical validation remain to be proven.
- Privacy/data concerns: As more sensitive health information is captured and processed (risk of hypertension, family history, etc.), users should be aware of how data is used, stored, and shared. Tom’s Guide emphasises reviewing privacy settings.
- Behavioural response matters: Even if the ring flags risk, the real health impact depends on users acting (e.g., verifying with a clinician, adjusting lifestyle). Merely having the alert doesn’t guarantee improved outcomes.
What this means for you as a user
- If you are an Oura Ring user and eligible: you may see a notification in your app offering you to join the study.
- Even if you don’t join: once the broader rollout happens, you can anticipate a new kind of feature in your “Vitals” or “My Health” tabs (as described in the redesign) that gives you a BP-risk category.
- Keep wearing your ring consistently (night & day if possible), make sure firmware/app are updated, and answer any questionnaires carefully — better data yields better algorithmic predictions.
- Consider using this as a prompt for real health checks: If your ring flags “major signs,” don’t ignore it — follow up with your doctor or a certified blood-pressure measurement.
- Remember: It’s a tool in addition to standard medical care — it doesn’t replace a cuff measurement, a clinician’s evaluation, or lifestyle/medication as directed by a health professional.
How this fits into the broader wearable-health ecosystem
From steps to biometrics to cardiovascular risk
We’ve witnessed wearables evolve: at first they counted steps; then heart-rate; then sleep and HRV; then ECGs and SpO₂; now we’re seeing blood pressure/hypertension monitoring creeping in.
The challenge always has been accuracy, regulatory clearance, and meaningful health-outcome impact. Measuring blood pressure reliably without a cuff is technically challenging (arterial pulse waveform, peripheral vasculature, calibration drift etc.). Yet the promise is significant: a wearable that can flag hypertension risk could transform preventive care.
Wearables in preventive health
Oura’s positioning emphasises a shift from “sick-care” to “preventive-care” — meaning identifying risks before they become acute events. Their press release says:
“Our goal is to make preventive health accessible and actionable for everyone. By combining rigorous research with continuous, real-world data, we can identify early patterns that often go unnoticed in traditional healthcare settings.”
In that sense, the Blood Pressure Profile Study is a gutsy move: it aligns with the vision that everyday wearables will one day serve as health-sentinels, not just lifestyle trackers.
Competitive dynamics
As mentioned, other major wearable makers (Apple, Samsung, Garmin, etc.) are racing toward blood-pressure or hypertension detection. Oura is differentiating itself by using a ring form factor, which may be more comfortable, unobtrusive, and suitable for continuous overnight wear — a prime environment for capturing subtle signals (sleep, HRV, micro-motions).
If Oura can pull off a credible BP-risk feature, it potentially gives them a meaningful competitive edge in the “smart ring” space and wearable health more broadly.
What to watch for next
To assess how this plays out, here are key milestones and questions to keep an eye on.
- Study rollout and participation numbers: How many users take part? What’s the demographic spread (age, sex, ethnicity, health status)? Broad participation improves the robustness of the algorithm’s generalisability.
- Published results / validation: Will Oura publish peer-reviewed data showing how well the algorithm’s risk flags correlate with “ground-truth” blood–pressure measurements? What are the sensitivity/specificity numbers?
- Regulatory clearance/label: Will this feature undergo FDA clearance (or equivalent outside the U.S.) and what claims will it be allowed to make?
- Feature rollout & user interface: When will the risk feature go from “study only” to “public rollout”? How will it appear in the app? What kind of user experience (UI/UX) will it offer — for example, education, warnings, next steps, integration with clinician follow-up?
- Data privacy & sharing: How will Oura handle this more sensitive health-risk data? Will users be required to consent to more detailed data capture? Will there be transparency about algorithms and data usage?
- Real-world impact: Ultimately, does the feature lead to measurable changes in behaviour (medical follow-up, lifestyle changes) and improved health outcomes? Many health-tech features are promising but fail at the “last mile” of behavioural impact.
Scenarios: best case / typical case / worst case
Best-case scenario
- Oura’s algorithm proves accurate (e.g., flags most people who have or will develop hypertension, with few false positives).
- The feature obtains regulatory clearance or at least public rollout.
- Users receive meaningful risk alerts, follow up with clinicians, adjust lifestyle early, and as a result the incidence of undiagnosed hypertension decreases.
- Oura distinguishes itself in the market and broadens the wearables-for-health narrative.
Typical/realistic scenario
- The algorithm works reasonably well (moderate sensitivity), but there are limitations: false positives/negatives, some demographic groups less well covered.
- Oura rolls out a “risk category” feature without full diagnostic claims (which is more likely).
- Some users act on the alerts, but many treat them as general awareness (without immediate medical follow-up).
- The feature becomes a nice addition to Oura’s ecosystem, but not a wholesale disruptive leap in hypertension diagnosis.
Worst-case scenario
- The algorithm performs poorly (e.g., too many false positives, limited correlation with actual BP readings).
- Regulatory issues or consumer trust problems emerge.
- The feature is delayed or reduced in scope.
- Users ignore the risk alerts, or worse, misinterpret them and avoid proper medical care.
- Rather than helping prevention, the feature becomes noise or marketing hype.
Practical advice for users — today
- Stay grounded: If you wear an Oura Ring, continue to use it for sleep, readiness, recovery, activity — those features are proven and useful. But don’t rely solely on any forthcoming BP-risk feature as a medical decision-maker.
- Keep your ring updated: Firmware + app updates are essential for accuracy of new features.
- Answer the questionnaires honestly: The study uses family history, medications, lifestyle habits — your input matters.
- Maintain a standard BP-monitoring routine (if you are concerned about blood pressure). Wearables supplement, not replace, traditional measurements.
- Interpret risk alerts wisely: If/when you receive a “Major signs” flag, it should prompt a clinician check-in — not panicking, but proactive follow-up.
- Think about lifestyle: Hypertension risk is modifiable. Use any risk insights as motivation to optimise sleep, reduce stress, move more, improve diet.
- Review privacy settings: As wearable health becomes more advanced, ensure you control how your data is shared and retained.
Broader implications: Why this could be a turning point
If Oura succeeds, we could reach a tipping point in wearable health: where rings (and other unobtrusive devices) move from simply tracking a few metrics to becoming early-warning systems for chronic, silent conditions such as hypertension, atrial fibrillation, sleep apnea, etc.
For healthcare systems, that means potential for earlier intervention, lower long-term costs, and improved outcomes. For consumers, that means something you wear at night might flag risk before your doctor’s annual check-up does.
However, the pathway is not simple. Accuracy, regulatory compliance, data integrity, user behaviour, and follow-through all matter. And worst case, wearables may overpromise and underdeliver, leaving users disappointed or confused.
But the fact that Oura is investing in a formal, IRB-approved study signals seriousness. They’re not just adding a “blood pressure” slider; they’re building a research-backed feature and aligning with regulatory frameworks. That’s encouraging.
Final thoughts
The announcement of the Blood Pressure Profile Study by Oura Labs is more than just a new feature teased for marketing. It represents a bold step in the convergence of consumer wearables and cardiovascular health monitoring.
If you’re an Oura Ring user (or considering becoming one), this is a development worth watching. While the study is U.S.-limited for now and the feature is investigational rather than diagnostic, the potential upside is meaningful. The ability to passively monitor subtle physiological signals and flag elevated blood-pressure risk could reshape how we think about preventive health in everyday life.
That said, cautious optimism is appropriate. Wearables are powerful tools, but they are just tools — they don’t replace medical advice, diagnosis, or treatment. The true health outcome of this initiative will depend not only on the algorithm’s accuracy but on user action, medical follow-up, and integration into broader healthcare frameworks.




