What Are the Effective Treatments of Hidradenitis Suppurativa?
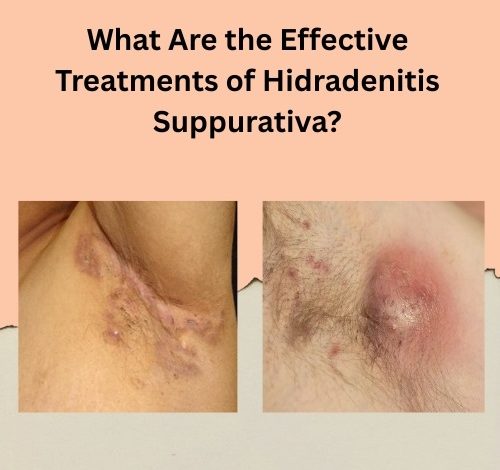
Hidradenitis Suppurativa (HS) is a chronic, inflammatory skin condition marked by painful lumps under the skin, typically in areas where skin rubs together, such as the armpits, groin, buttocks, and breasts. These lumps can break open, draining pus and forming tunnels under the skin. The disease is not just physically painful—it can also significantly affect a patient’s quality of life, mental well-being, and social interactions.
Understanding the effective treatments of hidradenitis suppurativa is vital for controlling symptoms, minimizing flare-ups, and improving patients’ overall well-being. While there is no known cure for HS, numerous medical, surgical, and lifestyle approaches can significantly alleviate symptoms and slow progression. This article explores these treatment options in detail, providing a comprehensive guide for patients and caregivers alike.
Understanding Hidradenitis Suppurativa
Before diving into treatments, it’s important to grasp the nature of the disease. HS is thought to be caused by an abnormal response of the immune system that leads to inflammation around hair follicles. It typically starts after puberty and is more common in women. Factors such as genetics, hormonal imbalances, obesity, smoking, and metabolic syndrome can all play a role in triggering or worsening the condition.

The disease is categorized into three stages (Hurley stages):
- Stage I: Single or multiple abscesses without sinus tracts or scarring
- Stage II: Recurrent abscesses with sinus tracts and scarring
- Stage III: Diffuse or multiple interconnected tracts and abscesses across a large area
Early diagnosis and timely intervention are essential for successful management.
Medical Treatments of Hidradenitis Suppurativa
1. Topical Treatments
Topical therapies are often the first line of treatment for mild HS cases (Hurley Stage I).
- Clindamycin 1% topical solution is commonly prescribed. It helps reduce bacterial growth and inflammation.
- Resorcinol cream (15%), a keratolytic agent, may help break down keratin plugs and reduce pain and inflammation.
These are generally safe for long-term use and may help prevent the progression of the disease.
Related Article: Does Laser Hair Removal Help Hidradenitis Suppurativa
2. Oral Antibiotics
Antibiotics serve a dual role in HS management: combating infection and reducing inflammation.
- Tetracyclines (doxycycline, minocycline) are typically prescribed for moderate disease.
- Clindamycin and Rifampin combination therapy has been effective in reducing lesions and promoting healing in more advanced stages.
- Metronidazole may be used for its anti-inflammatory and antimicrobial properties.
Treatment duration can range from a few weeks to several months, depending on disease severity.
3. Biologic Therapy
Biologics are among the most effective treatments of hidradenitis suppurativa, especially in moderate to severe cases (Hurley Stages II and III).
- Adalimumab (Humira) is the only FDA-approved biologic for HS. It’s a TNF-alpha inhibitor that reduces inflammation and prevents new lesions.
- Other biologics like infliximab, ustekinumab, and secukinumab are being studied for off-label use with promising results.
Biologics are administered via injections and can lead to significant symptom relief and prolonged remission, although they are costly and may cause side effects.
Related Article: Natural Relief for Hidradenitis Suppurativa: Top 6 Herbal Remedies
4. Hormonal Therapy
- Oral contraceptives (especially those containing estrogen and anti-androgens like cyproterone acetate) may help regulate hormonal levels.
- Spironolactone, an anti-androgen, has been found effective in some women with hormonally driven HS.
- Finasteride, commonly used in men, has shown some benefits in HS management by blocking dihydrotestosterone (DHT).
5. Corticosteroids
Systemic and intralesional corticosteroids may be used during acute flares:
- Oral prednisone can quickly reduce inflammation but is not suitable for long-term use due to side effects.
- Intralesional steroid injections may help shrink individual nodules.
These are short-term options and should be used under strict medical supervision.
6. Immunosuppressive Drugs
Drugs like cyclosporine, methotrexate, and azathioprine have been used in refractory HS cases. These drugs suppress immune system activity and are generally reserved for patients who don’t respond to first-line therapies.
Related Article: Herbal Products and Natural Remedies for Hidradenitis Suppurativa
Surgical Treatments of Hidradenitis Suppurativa
When medical therapy fails or when the disease reaches advanced stages, surgery may offer the most definitive relief.
1. Incision and Drainage (I&D)
This minor procedure can provide immediate relief during acute flares. However, it is not a long-term solution as it does not remove the sinus tracts or prevent recurrence.
2. Deroofing
Deroofing is a technique where the “roof” of the tunnels under the skin is removed, allowing the wound to heal from the base.
- Suitable for Hurley Stage I and II
- Less invasive than excision
- Often combined with laser therapy
3. Wide Excision
This involves surgically removing all affected skin and tissue in an area.
- Highly effective in preventing recurrence
- Commonly used in Hurley Stage III
- May require skin grafts or flap closures
Healing time can be significant, but results are generally durable.
4. Laser Therapy
Carbon dioxide (CO2) laser and Nd:YAG laser can be used to ablate diseased tissue and hair follicles.
- Effective for reducing lesion count and recurrence
- Often combined with deroofing or excision
- Minimal scarring
Laser therapy is gaining popularity due to its precision and minimally invasive nature.
Related Article: Hidradenitis Suppurativa Symptoms, Causes, Diagnosis and Treatment
Lifestyle Modifications and Natural Remedies
1. Weight Management
Obesity is a major risk factor and aggravator for HS. Reducing weight through a balanced diet and regular exercise can significantly decrease flare-ups.
- Anti-inflammatory diets (rich in fruits, vegetables, lean protein, and whole grains) are beneficial
- Reducing dairy, refined sugars, and processed foods may help
2. Smoking Cessation
Smoking is strongly associated with the development and worsening of HS. Quitting smoking can dramatically reduce symptoms over time.
3. Proper Hygiene and Skin Care
- Use antibacterial or antiseptic cleansers like chlorhexidine
- Avoid harsh soaps and friction
- Wear loose-fitting, breathable clothing
- Apply warm compresses during flares
4. Stress Management
Stress can worsen inflammation and trigger flares. Incorporating practices like meditation, yoga, and adequate sleep can be helpful adjuncts to medical treatment.
Emerging and Alternative Treatments of Hidradenitis Suppurativa
1. Zinc Gluconate Supplements
Zinc has anti-inflammatory properties and may help reduce lesion formation. It’s particularly useful in mild to moderate HS, often as an adjunct therapy.
2. Turmeric and Curcumin
Turmeric’s active ingredient, curcumin, has shown anti-inflammatory benefits. Some patients report reduced pain and fewer flare-ups with daily supplementation.
3. Probiotics and Gut Health
A healthy gut microbiome may help regulate immune responses and reduce systemic inflammation. Probiotic supplements and fermented foods are often recommended.
4. Botulinum Toxin (Botox)
Some small studies have shown promise in using Botox to reduce sweating and inflammation in HS-affected areas. This approach is still experimental but may be an option in specific cases.

Mental Health and Psychosocial Support
HS has a profound emotional and psychological impact. Patients may suffer from:
- Depression
- Anxiety
- Social isolation
- Low self-esteem
Incorporating mental health care into the treatment plan is crucial:
- Cognitive-behavioral therapy (CBT)
- Support groups (online or in-person)
- Mindfulness-based stress reduction (MBSR)
Addressing the emotional aspect of HS can significantly improve overall quality of life.
Customized Treatment Plans: One Size Doesn’t Fit All
The most effective treatments of hidradenitis suppurativa depend on multiple factors:
- Disease severity (Hurley stage)
- Location and extent of lesions
- Response to past treatments
- Presence of other medical conditions
- Patient preferences
A multidisciplinary team—including dermatologists, surgeons, psychologists, and nutritionists—often works together to develop personalized care plans for each individual.
Conclusion: Managing HS Is a Journey, Not a Destination
While hidradenitis suppurativa is a chronic and often debilitating condition, many treatments of hidradenitis suppurativa can offer significant relief. From antibiotics and biologics to surgical options and lifestyle changes, a combination approach often yields the best results. Early diagnosis, individualized treatment, and comprehensive care are key to helping patients manage their condition and live fuller, more comfortable lives.
If you or someone you know suffers from HS, consult a dermatologist to discuss the most appropriate treatment strategy. With ongoing research and emerging therapies, hope continues to grow for those affected by this challenging condition.